Salesforce HIPAA Compliance
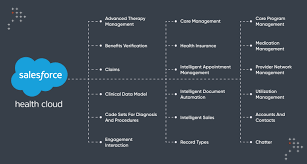
Compliance plays a critical role in managing sensitive information, especially under regulations like the Health Insurance Portability and Accountability Act (HIPAA). Salesforce HIPAA Compliance. Enacted in 1996, HIPAA establishes national standards for safeguarding sensitive health information. Organizations and individuals who store, manage, or transmit healthcare data are subject to these regulations, which prioritize the confidentiality, integrity, and availability of patient information. While Salesforce provides tools to support HIPAA compliance, the responsibility for ensuring compliance ultimately lies with the data-processing organization or individual—not solely the platform itself. This insight explores Salesforce’s role in HIPAA compliance, key features for safeguarding electronic Protected Health Information (ePHI), and best practices for adhering to regulatory requirements. Understanding HIPAA Salesforce’s flexibility as a CRM platform allows it to serve industries that require HIPAA compliance, particularly healthcare and life sciences. At its core, HIPAA protects Protected Health Information (PHI)—any patient-identifiable information in medical records. PHI extends beyond traditional medical data to include names, addresses, birth dates, Social Security numbers, and more. When PHI is managed or transmitted electronically, it’s classified as electronic Protected Health Information (ePHI), which is subject to additional safeguards. Entities Covered by HIPAA HIPAA applies to several types of entities: While Salesforce is classified as a Business Associate, organizations using the platform remain responsible for adhering to HIPAA’s security requirements. Salesforce and the Business Associate Agreement (BAA) As a Business Associate, Salesforce must enter into a Business Associate Agreement (BAA) with healthcare organizations and other Covered Entities to define responsibilities and security measures for handling ePHI. The BAA outlines the Salesforce features and services eligible for HIPAA compliance. Notably: Without a signed BAA, organizations face significant penalties for HIPAA violations, even in the absence of a data breach. HIPAA-Compliant Salesforce Solutions Salesforce offers various solutions and features to support HIPAA compliance. These are categorized into platform security measures and specific compliant services: Key Security Features HIPAA-Compliant Services It’s important to note that not all Salesforce features are HIPAA-compliant, and proper configuration is critical to ensure compliance. Restrictions and Challenges While Salesforce offers robust security tools, some limitations and risks exist: Additionally, some Salesforce services, like certain social or mobile features in Health Cloud, are not compliant by default and require explicit mention in the BAA to be used with ePHI. Best Practices for HIPAA Compliance To maximize HIPAA compliance with Salesforce, organizations should: HIPAA Compliance Checklist Here’s a concise checklist to guide your HIPAA compliance efforts: Leveraging Third-Party Tools Solutions like GRAX can enhance HIPAA compliance in Salesforce by adding capabilities such as data backup, archiving, and recovery. GRAX’s security features include: However, integrating third-party solutions requires careful vetting to avoid compliance risks. Salesforce HIPAA Compliance Salesforce is a powerful tool for healthcare organizations, but achieving HIPAA compliance requires understanding its capabilities and limitations. A well-configured Salesforce environment, combined with diligent user management and third-party tools, can help organizations meet regulatory requirements while safeguarding patient data. By embracing best practices and staying informed about shared responsibilities, organizations can ensure HIPAA compliance, avoid penalties, and build trust with patients and stakeholders. Like Related Posts Salesforce OEM AppExchange Expanding its reach beyond CRM, Salesforce.com has launched a new service called AppExchange OEM Edition, aimed at non-CRM service providers. Read more The Salesforce Story In Marc Benioff’s own words How did salesforce.com grow from a start up in a rented apartment into the world’s Read more Salesforce Jigsaw Salesforce.com, a prominent figure in cloud computing, has finalized a deal to acquire Jigsaw, a wiki-style business contact database, for Read more Health Cloud Brings Healthcare Transformation Following swiftly after last week’s successful launch of Financial Services Cloud, Salesforce has announced the second installment in its series Read more