AdventHealth Pioneers AI-Powered Denials Prevention Strategy
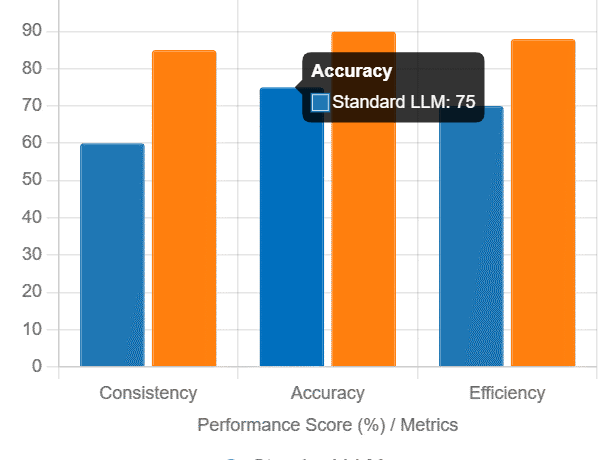
Transforming Denials Management from Reactive to Proactive While many health systems struggle with claim denial rates as high as 20%, AdventHealth is taking an innovative approach—using artificial intelligence to prevent denials before they occur. The Florida-based health system has implemented AI-driven tools that analyze medical documentation for potential issues prior to claim submission, creating a more efficient revenue cycle and better patient experience. “By identifying documentation gaps early, we’re able to address them before they become claim denials,” said Dr. Christopher Riccard, Vice President of Hospital Medicine and Clinical Documentation Integrity at AdventHealth. “This proactive approach helps us reduce delays and confusion for patients while protecting our revenue stream.” The High Cost of Claim Denials Claim denials represent more than just an administrative headache: “Denials don’t just hurt hospitals—they impact patients directly,” Riccard emphasized. “Our goal is to ensure accurate, timely billing so patients understand their financial responsibility without unnecessary delays.” How AI Prevents Denials Before They Happen AdventHealth’s partnership with Iodine Software has yielded a cutting-edge solution: Key results include: Building an Intelligent Revenue Cycle Ecosystem AdventHealth views AI-powered denials prevention as just the beginning. The health system is exploring broader applications of AI across the revenue cycle: Emerging Technologies in Action Human-Centered Implementation Riccard stresses that technology alone isn’t the solution: “Success requires thoughtful integration into existing workflows. We worked closely with our clinical teams to ensure these tools actually solve real problems rather than create new ones.” The Future of Revenue Cycle Management AdventHealth’s strategy represents a paradigm shift in healthcare finance: As Riccard notes: “Our ultimate goal is creating a self-correcting revenue cycle that supports both financial health and patient experience—where potential issues are identified and resolved almost before they emerge.” The health system’s approach demonstrates how AI, when implemented strategically, can transform one of healthcare’s most persistent challenges into an opportunity for improvement across clinical, financial, and patient experience domains. Like Related Posts Salesforce OEM AppExchange Expanding its reach beyond CRM, Salesforce.com has launched a new service called AppExchange OEM Edition, aimed at non-CRM service providers. Read more The Salesforce Story In Marc Benioff’s own words How did salesforce.com grow from a start up in a rented apartment into the world’s Read more Salesforce Jigsaw Salesforce.com, a prominent figure in cloud computing, has finalized a deal to acquire Jigsaw, a wiki-style business contact database, for Read more Service Cloud with AI-Driven Intelligence Salesforce Enhances Service Cloud with AI-Driven Intelligence Engine Data science and analytics are rapidly becoming standard features in enterprise applications, Read more