The Evolution Beyond AI Agents
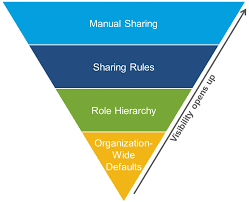
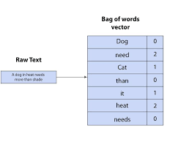
The Evolution Beyond AI Agents: What Comes Next? The Rapid Progression of AI Terminology The landscape of artificial intelligence has undergone a remarkable transformation in just three years. What began with ChatGPT and generative AI as the dominant buzzwords quickly evolved into discussions about copilots, and most recently, agentic AI emerged as 2024‘s defining concept. This accelerated terminology cycle mirrors fashion industry trends more than traditional technology adoption curves. Major players including Adobe, Qualtrics, Oracle, OpenAI, and Deloitte have recently launched agentic AI platforms, joining earlier entrants like Microsoft, AWS, and Salesforce. This rapid market saturation suggests the industry may already be approaching the next conceptual shift before many organizations have fully implemented their current AI strategies. Examining the Staying Power of Agentic AI Industry analysts present diverging views on the longevity of the agentic AI concept. Brandon Purcell, a Forrester Research analyst, acknowledges the pattern of fleeting AI trends while recognizing agentic AI’s potential for greater staying power. He cites three key factors that may extend its relevance: Klaasjan Tukker, Adobe’s Senior Director of Product Marketing, draws parallels to mature technologies that have become invisible infrastructure. He predicts agentic AI will follow a similar trajectory, becoming so seamlessly integrated that users will interact with it as unconsciously as they use navigation apps or operate modern vehicles. The Automotive Sector as an AI Innovation Catalyst The automotive industry provides compelling examples of advanced AI applications that transcend current “agentic” capabilities. Modern autonomous vehicles demonstrate sophisticated AI behaviors including: These implementations suggest that what the tech industry currently labels as “agentic” may represent only an intermediate step toward more autonomous, context-aware systems. The Definitional Challenges of Agentic AI The technology sector faces significant challenges in establishing common definitions for emerging AI concepts. Adobe’s framework describes agents as systems possessing three core attributes: However, as Scott Brinker of HubSpot notes, the term “agentic” risks becoming overused and diluted as vendors apply it inconsistently across various applications and functionalities. Interoperability as the Critical Success Factor For agentic AI systems to deliver lasting value, industry observers emphasize the necessity of cross-platform compatibility. Phil Regnault of PwC highlights the reality that enterprise environments typically combine solutions from multiple vendors, creating integration challenges for AI implementations. Three critical layers require standardization: Without such standards, organizations risk creating new AI silos that mirror the limitations of legacy systems. The Future Beyond Agentic AI While agentic AI continues its maturation process, the technology sector’s relentless innovation cycle suggests the next conceptual breakthrough may emerge sooner than expected. Historical naming patterns for AI advancements indicate several possibilities: As these technologies evolve, they may shed specialized branding in favor of more utilitarian terminology, much as “software bots” became normalized after their initial hype cycle. The automotive parallel suggests that truly transformative AI implementations may become so seamlessly integrated that their underlying technology becomes invisible to end users—the ultimate measure of technological maturity. Until that point, the industry will likely continue its rapid cycle of innovation and rebranding, searching for the next paradigm that captures the imagination as powerfully as “agentic AI” has in 2024. Like Related Posts Salesforce OEM AppExchange Expanding its reach beyond CRM, Salesforce.com has launched a new service called AppExchange OEM Edition, aimed at non-CRM service providers. Read more The Salesforce Story In Marc Benioff’s own words How did salesforce.com grow from a start up in a rented apartment into the world’s Read more Salesforce Jigsaw Salesforce.com, a prominent figure in cloud computing, has finalized a deal to acquire Jigsaw, a wiki-style business contact database, for Read more Service Cloud with AI-Driven Intelligence Salesforce Enhances Service Cloud with AI-Driven Intelligence Engine Data science and analytics are rapidly becoming standard features in enterprise applications, Read more