AI’s Potential to Reduce Provider Burdens in the Prior Authorization Process
Artificial intelligence (AI) has the potential to significantly ease the documentation and substantiation burdens providers face during the prior authorization process. Prior authorization, a critical step where health plans approve or deny coverage for services or prescriptions before they’re administered, is a key cost-control mechanism in the U.S. healthcare system. While it helps payers avoid unnecessary spending, the process poses significant challenges, especially for healthcare providers tasked with gathering and submitting documentation. AI Potential to Improve Prior Authorizations examined.
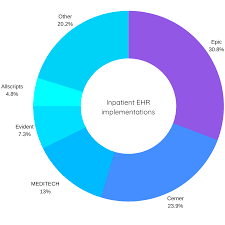
Historically, prior authorization has been a major regulatory challenge for providers, surpassing other issues such as electronic health record (EHR) interoperability and compliance with the No Surprises Act. Despite its cumbersome nature, prior authorization isn’t likely to be eliminated, as it plays a crucial role in balancing healthcare affordability and access to quality care.
AI Potential to Improve Prior Authorizations
The transactional nature of many prior authorization tasks makes them ripe for automation. Increasingly, stakeholders are turning to AI and other technology-driven solutions to streamline the process, making it less burdensome for providers.
How AI Can Streamline Prior Authorization
AI has already been applied to various aspects of healthcare, from automating hospital discharges to alleviating the administrative burdens of nurses. When applied to prior authorization, AI can speed up the approval process for both providers and payers, reducing delays in patient care and lowering administrative costs.
Health insurance companies are already beginning to leverage AI to expedite prior authorization and claims decisions. However, concerns are growing over whether the use of AI in these areas complies with state and federal regulations. For example, a 2023 AMA Annual Meeting resolution cited an investigation revealing that Cigna doctors denied over 300,000 claims in two months, spending an average of just 1.2 seconds per case using AI.
UnitedHealthcare has also employed AI to make “fast, efficient, and streamlined coverage decisions,” raising questions about whether these decisions adhere to regulatory standards for fairness and accuracy.
AMA’s Call for Oversight on AI in Prior Authorization
Recognizing the risks, the American Medical Association (AMA) has called for increased regulatory oversight of AI in prior authorization. Specifically, the AMA advocates for:
- Ensuring AI reviews are based on accurate clinical criteria from national medical specialty guidelines and peer-reviewed literature.
- Requiring reviews by unbiased healthcare professionals with relevant expertise.
- Mandating that human reviews of patient records occur before care is denied.
AI could potentially reduce the time-consuming, manual tasks associated with prior authorization. However, as AMA Trustee Dr. Marilyn Heine cautioned, “AI is not a silver bullet.” The increasing reliance on AI for prior authorization must not add to the already overwhelming volume of requirements that burden physicians and hinder patient care. Nor can it increase the threat of cyberattacks.
Fixing Prior Authorization: AMA’s Role
Addressing the challenges of prior authorization is a key part of the AMA’s Recovery Plan for America’s Physicians. The organization is committed to reducing the overuse of prior authorization and improving the fairness of existing processes, ensuring that the use of AI in healthcare supports—not hinders—patient care. To that end, the AMA continues to research the costs and impacts of prior authorization on healthcare providers and patients.
To learn more about the proper use of AI in medicine and the AMA’s efforts to reform prior authorization, visit the AMA’s resources on healthcare AI.
Content updated September 2024.